Introduction
Cervicogenic headaches are a common and often debilitating type of headache that originates in the cervical spine or neck region. With the growing prevalence of sedentary lifestyles and poor posture, more and more people are experiencing these types of headaches, making the need for effective treatment options even greater. At Impact Physical Therapy, our skilled therapists use evidence-based manual physical therapy techniques to alleviate the pain associated with cervicogenic headaches and improve patients’ overall quality of life. In this comprehensive blog post, we’ll take an in-depth look at the diagnosis of cervicogenic headaches and explore the effectiveness of manual physical therapy techniques in their treatment.
Understanding Cervicogenic Headaches
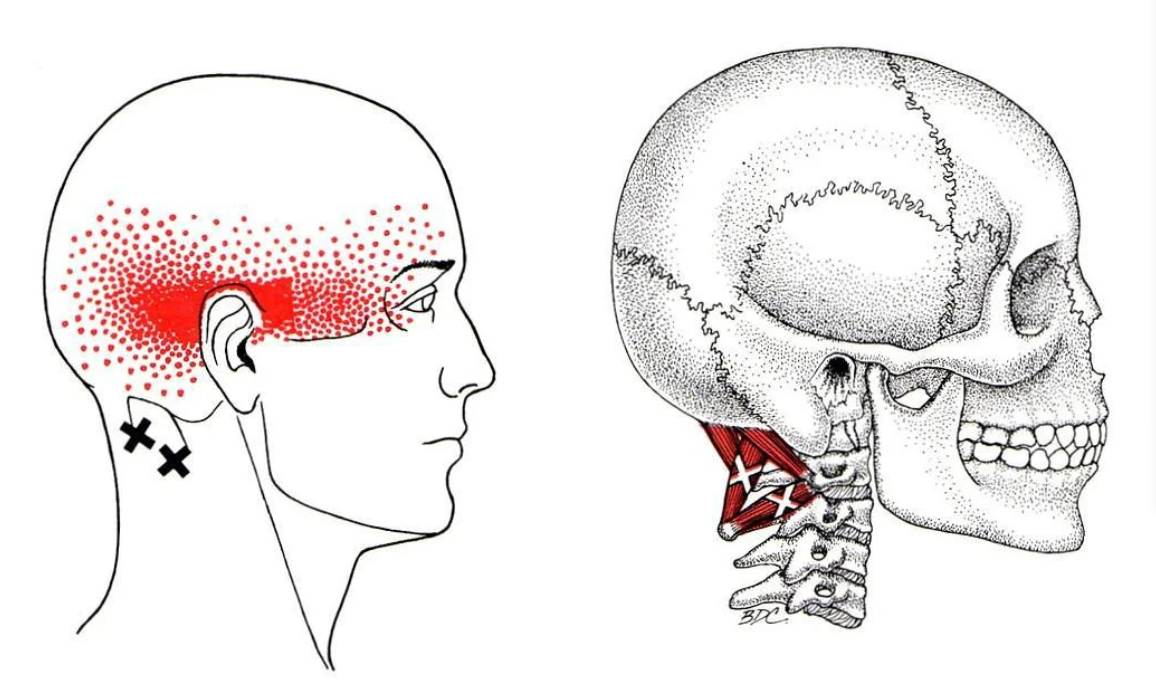
Cervicogenic headaches are secondary headaches that originate in the cervical spine or neck region, specifically the upper three cervical vertebrae (C1, C2, and C3) and their surrounding structures such as joints, ligaments, muscles, and nerves. These headaches are characterized by pain that begins at the base of the neck or skull and radiates toward the front of the head, usually following a specific pattern depending on the affected neck structures.
Cervicogenic headaches are usually caused by dysfunction or injury to the cervical spine, including the cervical vertebrae, joints, ligaments, or neck muscles. Common influencing factors include.
-Bad posture: Slouching or maintaining incorrect head and neck posture for long periods of time can strain the muscles and joints of the cervical spine.
-Whiplash injuries: Rapid acceleration and deceleration of the head in a motor vehicle accident can damage the structures of the neck and lead to cervicogenic headaches.
-Degenerative diseases: Diseases such as osteoarthritis, disc degeneration, or spinal stenosis can lead to changes in the cervical spine that can cause cervicogenic headaches.
-Muscle tension: Chronic muscle tension in the neck and upper back can lead to cervicogenic headaches.
Symptoms of cervicogenic headaches vary from person to person, but usually include.
- Unilateral pain: Cervicogenic headaches usually cause pain on one side of the head, although the pain can sometimes shift to one side or affect both sides. 2.
- Site and pattern of pain: Pain usually begins at the base of the skull or neck and then radiates to the front of the head, with a specific pattern depending on the cervical structures affected. It may also extend to the shoulders, upper back, or the affected arm.
- Intensity and quality of pain: The intensity of the pain varies from mild to severe and is often described as a constant dull ache or sharp stabbing sensation. Certain neck movements or sustained neck postures, such as looking up, down, or to the side for long periods of time, may exacerbate the pain.
- Reduced neck mobility: Patients with cervicogenic headaches often experience stiffness and limited range of motion in the neck, which may exacerbate the headache.
- Associated Symptoms: Some people with cervicogenic headaches may also experience other symptoms such as nausea, dizziness, blurred vision, sensitivity to light or sound, or difficulty concentrating. However, these symptoms are less common in cervicogenic headaches than in other types of headaches, such as migraines.
Diagnosing cervicogenic headaches
Diagnosing cervicogenic headaches can be challenging because their symptoms often overlap with other types of headaches, such as migraines and tension headaches. However, an accurate diagnosis is critical to providing appropriate treatment and achieving lasting relief. The diagnostic process for cervicogenic headaches typically includes the following steps.
- Detailed history: The first step in diagnosing cervicogenic headaches is a thorough medical history. The therapist will ask about the patient’s symptoms, medical history, and any factors or triggers that may be contributing to the headache.
- Physical Examination: The therapist will perform a thorough physical examination, focusing on the patient’s cervical spine, neck muscles and posture. They will assess the patient’s range of motion, muscle strength, and any pressure or pain in the neck and upper back.
- Diagnostic Imaging: In some cases, diagnostic imaging, such as x-rays, MRIs, or CT scans, can be used to identify potential problems in the cervical spine that may be causing the patient’s headaches.
- Diagnostic Nerve Blocks: Diagnostic nerve blocks may be used to confirm the diagnosis of cervicogenic headaches. This involves injecting a local anesthetic into specific nerves or structures in the neck to temporarily block pain signals. If the headache is significantly reduced or eliminated after the injection, the diagnosis of cervicogenic headache is supported.
Manual Physical Therapy Techniques for Cervicogenic Headaches

At Impact Physical Therapy, we use a variety of evidence-based manual physical therapy techniques to effectively treat cervicogenic headaches. The goal of manual therapy is to address the underlying cause of the headache by improving joint mobility, muscle flexibility, and overall function of the cervical spine. Some of the common manual physical therapy techniques used by Impact Physical Therapy to treat cervicogenic headaches include.
-Joint mobilization: This technique involves applying controlled gentle force to the cervical spine joints to improve their mobility and reduce pain. Joint mobilization can help relieve joint stiffness, restore normal joint function, and reduce muscle tension that causes cervicogenic headaches.
-Soft Tissue Activities: Soft tissue activities focus on releasing tightness and adhesions in the muscles, fascia and other soft tissues around the cervical spine. This can be accomplished through techniques such as massage, manual stretching, or instrument-assisted soft tissue mobilization (IASTM). By relieving soft tissue tension, patients can reduce headaches and improve neck function.
Myofascial Release: Myofascial release is a special form of soft tissue activity that targets the connective tissue (fascia) that surrounds and supports the muscles. The technique involves applying sustained pressure to tight, restricted areas of fascia to release tension and improve tissue flexibility. Myofascial release has been shown to be effective in reducing pain and improving range of motion in patients with cervicogenic headaches.
Muscle Energy Technique (MET): MET is a manual therapy that utilizes the patient’s muscle contractions to improve joint mobility and muscle flexibility. The therapist guides the patient through specific, controlled muscle contractions, followed by relaxation and stretching.MET can be particularly helpful in addressing the muscle imbalances and joint restrictions that lead to cervicogenic headaches.
Evidence Supporting Manual Physical Therapy for Cervicogenic Headaches
Numerous studies have demonstrated the effectiveness of manual physical therapy techniques in the treatment of cervicogenic headaches. Example.
A 2014 systematic review published in the Journal of Orthopaedic and Sports Physical Therapy analyzed the evidence for manual therapy in the treatment of cervicogenic headache. The review concluded that there is strong evidence to support the use of joint mobilization, soft tissue movement, and myofascial release to reduce pain and improve function in patients with cervicogenic headache.
A randomized controlled trial published in 2016 in the journal BMC Musculoskeletal Disorders compared the effectiveness of manual therapy, exercise therapy, and a combination of the two for the treatment of cervicogenic headache. It found that all three treatments significantly improved headache, neck function and quality of life. However, the combination of manual therapy and exercise therapy produced the best results, emphasizing the importance of an integrated treatment approach.
A systematic review and meta-analysis published in the journal Physical Therapy in 2019 found that manual therapy, including joint mobilization and soft tissue activities, was effective in reducing headache and improving cervical spine function in patients with cervicogenic headache. The authors concluded that manual therapy should be considered a primary treatment option for these patients.
Combining manual physical therapy with other treatments
At Impact Physical Therapy, we recognize the importance of a comprehensive, multifaceted treatment approach to achieve the best possible outcomes in patients with cervicogenic headaches. In addition to manual physical therapy techniques, our therapists may incorporate the following interventions into a patient’s treatment plan:.
-Therapeutic exercises: Specific stretching and strengthening exercises that target the muscles of the neck and upper back help improve flexibility, reduce muscle tension, and support proper alignment of the cervical joints.
-Postural exercises: Addressing postural issues, such as forward head posture or rounded shoulders, is a key component of cervicogenic headache treatment. Our therapists provide education and instruction on proper posture and ergonomics in daily activities and tasks.
-Modalities: The use of modalities, such as heat, cold, ultrasound, or electrical stimulation, can provide temporary relief from headaches and muscle tension.
-Patient education: Keeping patients informed about their condition and self-management strategies is critical to the long-term success of treating cervicogenic headaches. Our therapists provide patients with information about headache triggers, relaxation techniques, and home exercise programs to support their ongoing recovery and prevent future headaches.
Conclusion
Cervicogenic headaches can severely impact an individual’s quality of life, making it critical to accurately diagnose and treat the underlying cause of the pain. At Impact Physical Therapy, our evidence-based approach to treating cervicogenic headache combines manual physical therapy techniques with therapeutic exercises, postural training, and patient education to provide comprehensive and effective care.
Research supports the use of manual physical therapy techniques such as joint mobilization, soft tissue mobilization, myofascial release, and muscle energy techniques to reduce pain and improve function in patients with cervicogenic headache. By addressing underlying issues in the cervical spine and surrounding soft tissues, our skilled therapists at Impact Physical Therapy can help patients achieve lasting headache relief and improve their overall quality of life.
Sources:
– Haas, M., Bronfort, G., & Evans, R. (2014). Spinal manipulative therapy and exercise for headaches: a systematic review. Journal of Orthopaedic & Sports Physical Therapy, 44(6), 428-438.
– Luedtke, K., Allers, A., Schulte, L. H., & May, A. (2016). Efficacy of interventions used by physiotherapists for patients with headache and migraine—systematic review and meta-analysis. Cephalalgia, 36(5), 474-492.
– Chaibi, A., Knackstedt, H., Tuchin, P. J., & Russell, M. B. (2016). Chiropractic spinal manipulative therapy for cervicogenic headache: a single-blinded, placebo, randomized controlled trial. BMC Musculoskeletal Disorders, 17(1), 1-9.
– Racicki, S., Gerwin, S., DiClaudio, S., Reinmann, S., & Donaldson, M. (2013). Conservative physical therapy management for the treatment of cervicogenic headache: a systematic review. Journal of Manual & Manipulative Therapy, 21(2), 113-124.



